A QI collaborative helped 31 small practices improve critical quality measures
Doing more with less. That could be the motto for the small, independent healthcare practices across the United States where around 75% of all Medicaid primary care visits happen each year.
With just a couple of exam rooms and a handful of staff members, small, independent practices provide some of the most culturally responsive, accessible, and cost-effective medical care in the U.S. And they often serve and build trust with historically marginalized groups who have the lowest trust in the healthcare system overall. This makes them powerful—and often overlooked—leverage points to improve health and health equity. If, that is, they get the support they need.
Small practices have limited resources and often struggle to stay afloat, which makes it more difficult to collect data and implement quality improvement (QI) initiatives that can improve health outcomes. However, a set of sites in California recently demonstrated that with the right support, even the smallest practices can achieve significant improvements in quality measures.
In 2023, 31 small practices joined Equity and Quality at Independent Practices in Los Angeles County (EQuIP-LA), a two-year QI collaborative funded by the California Health Care Foundation. It was designed to provide independent practices with some of the foundational knowledge, skills, and resources necessary for data collection and QI design, which have historically been cost-prohibitive and out of reach for organizations of their size. HealthBegins served as the health equity advisor for the collaborative.
Practices each received a modest grant, technical assistance, data analytics support, and hands-on coaching to design QI initiatives to address three quality measures: diabetes management, colorectal cancer screenings, and hypertension management. They reviewed critical organizational capabilities, identified their organizational strengths, and prioritized improvement opportunities across each target quality measure. Practices set clear, measurable goals to track their progress and designed and implemented tests of change to meet those goals. Health equity was embedded throughout EQuIP-LA’s design, from recruiting practices that serve diverse populations to incorporating patient and family engagement.
The effort led to statistically significant health improvements and highlighted lessons, as outlined below, that could help amplify the impact of small practices in advancing equity in more places.
Changes made by practices improved health.
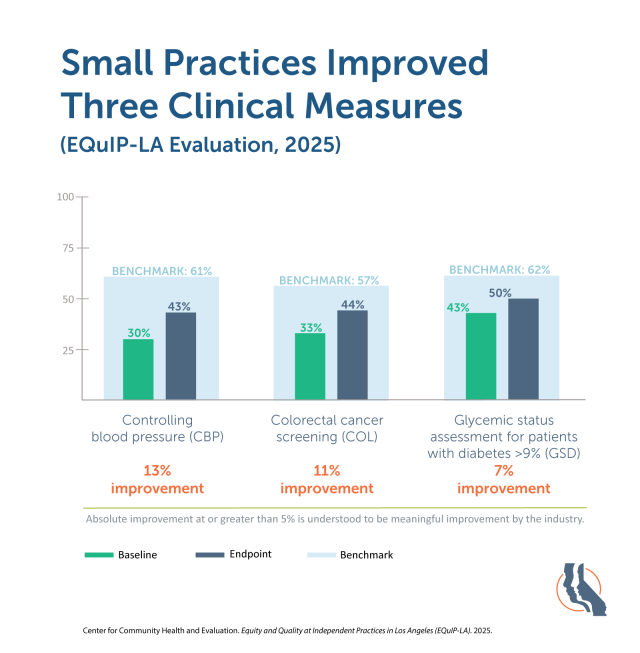
An evaluation of EQuIP-LA conducted by the Center for Community Health and Evaluation found that the changes small practices implemented significantly improved patients’ health. Thirty out of 31 practices improved on at least one quality measure, and most improved on more than one. Across all practices, there was a 13% improvement in controlling blood pressure and a 7% improvement in glycemic control among patients with diabetes. Colorectal cancer screening also increased by 11%. These improvements moved the small practices closer to reaching national quality benchmarks set by the Centers for Medicare & Medicaid Services. Most importantly, they translate to longer lives, earlier cancer detection, and overall better health for patients.
QI strategies worked because they were tailored to each small practice.
The QI initiatives implemented varied by practice. Each one was designed and led by staff, responding to their practice’s unique data, patient and community needs, and resources. Some of the effective strategies included tailored patient outreach, patient education, data stratification, improved workflow documentation, and at-home screening kits. For example, at Reddy Care Medical in Pomona, California, community health workers began proactively screening patients for social determinants of health and connecting them with resources to help meet their health and healthcare needs. In this video, Alex Hernandez III, Director of Business Development at Reddy Care, explained how that additional outreach made a difference for patients.
“We have the diabetic patient that we know needs to go to the lab every three months to have a hemoglobin A1c drawn,” said Hernandez. “So, we’re looking at all of that and saying, ‘Hey, our assessment says you need transportation. Does that mean you’re having a hard time going to get your lab work done? Yes? Okay, we gotta find a resource for that.’” By assigning a community health worker to help close that care gap, he said, “I know that we’re reducing hospitalization outright.”
Staff at Reddy Care emphasized that part of the reason this strategy was successful was that EQuIP-LA trained the community health workers already on staff, who were familiar with the practice’s workflows and patients, to perform this work. They were able to hit the ground running and conduct screenings in the languages their patients are most comfortable using.
Expanded capacity will allow practices to address future care gaps.
The goal of EQuIP-LA wasn’t only to improve the three target quality measures. It also focused on building capacity in small practices so that they can reduce future care gaps, especially by equipping them to better leverage QI tools. After participating in the collaborative, practices’ assessment scores notably improved across seven capabilities—engaged leadership, data-driven improvements, team-based care, patient-team partnership, population health management, access to care, and social drivers and community partners. Most practices achieved the maximum score in at least one domain.
Small practices weren’t the only organizations that built capacity. EQuIP-LA employed a train-the-trainer model, in which four provider organizations—Allied Pacific IPA, L.A. Care Health Plan, Angeles IPA, and Omnicare Medical Group—provided coaching to each small practice. The EQuIP-LA evaluation revealed that the coaching organizations expanded internal QI and data infrastructures, enhanced coaching skills, and deepened relationships with the small practices.
Small practices hold big promise, but need more support.
Despite the vital role they play in the healthcare ecosystem, small practices face additional pressure as healthcare providers and organizations increasingly consolidate under large, corporate umbrellas. But studies show that this consolidation increases healthcare costs and, in some cases, decreases quality. The EQuIP-LA program reveals that small practices, which already have high trust with communities and often provide more cost-effective care, can also meet or exceed national quality benchmarks even with their limited resources. And as health plans continue to look for ways to reduce costs and improve outcomes at the same time, supporting small practices in this QI work is one critical way to do that.
The EQuIP-LA evaluation report offered steps stakeholders across the country can take to support small practices in their communities.
For small, independent practices:
- Participate in programs like EQuIP-LA to prompt reflection, identify areas for improvement, and access necessary resources.
- Build relationships with health plans and independent practice associations (IPAs) to facilitate access to data and secure support in meeting and exceeding benchmarks.
For health plans and independent practice associations:
- Provide tailored support to help practices meet and exceed benchmarks.
- Provide individualized data and support to drive practice-level improvements.
- Enhance the availability and consistency of demographic data to facilitate stratification and address disparities.
- Align incentive programs with high-priority clinical quality measures to drive improvement.
For supporters of independent practices (e.g., philanthropy, technical assistance providers):
- Customize support to each practice’s context.
- Prioritize trust-building early in program implementation.
- Set realistic expectations, recognizing that many practices are early in their QI journey.
- Embed health equity from the start, with clear definitions and processes for how it is being operationalized in the program
—
Read the full evaluation report of EQuIP-LA.
HealthBegins is proud to be the health equity advisor for EQuIP-LA and work alongside our partners on this initiative: the California Quality Collaborative (lead technical assistance partner), the Center for Community Health and Evaluation (lead evaluator), PFCCpartners (patient and family engagement advisor), L.A. Care Health Plan, Health Net, and Mission Boom (communications partner). EQuIP-LA is funded by the California Health Care Foundation.
