
Aaron Boush
Community Health and Outreach Director
Planning and Community Development, Carilion Clinic
Advice for Upstreamists
“Relationships, relationships, relationships. Most importantly, genuine relationships with our community members where we can fully listen and really understand their shared experiences. Relationships with other community organizations and even other healthcare organizations. If we’re going to improve community health, we can’t go at it alone. And relationships within the hospital walls. As we shift from fee-for-service to value-based care, we have to learn how to look upstream. So forming those relationships internally to understand why this work is important and how it influences health outcomes is essential.”
The Big Idea
When something like the recent pandemic hits and the needs of your patients and community change overnight, how do you rapidly and effectively pivot to address those changing needs? And how do you approach that work equitably? Those were the questions Aaron Boush, Carilion Clinic’s community health and outreach director, was asking in 2020 when his department was called to help coordinate the health system’s efforts to vaccinate the community.
Carilion’s network of seven hospitals and 247 primary care and specialty practices throughout Roanoke and western Virginia provide care for nearly 1 million people. Prior to the pandemic, the Community Health and Outreach Department’s work largely revolved around delivering in-person health education classes in community spaces. Biometric screenings, community immunization events, Morningside Urban Farm programming, community health worker services, and a peer recovery program were part of the department’s regular schedule.
Then, suddenly, Boush and his department were tasked with coordinating hundreds of staff members from the health system per day to support operations at the city health department’s mass vaccination centers. But it quickly became evident that most people receiving the vaccine at those clinics were White, and the organizations’ focus became ensuring more equitable distribution. They used city health department data to identify two Roanoke neighborhoods—both medically underserved with high rates of poverty and large communities of color—where vaccination rates were lowest. Then they worked closely with community leaders to identify barriers to vaccine access and strategies to get those communities vaccinated.
Along the way, Carilion learned that its ability to quickly and effectively develop an approach to distribute vaccines equitably relied on three factors: (1) the strength of the community relationships it had prior to the pandemic; (2) its ability to reduce silos within its organization and better coordinate the work of all staff; and (3) adapting a consistent, proven assessment tool to the situation.
The Details
Aaron Boush’s Origin Story
Aaron Boush’s career in health care started earlier than most. Inspired by his grandmother, a retired hospital leader and volunteer, Boush spent almost every Saturday and Sunday as a teen volunteering at a local hospital. By the time he graduated from high school, he’d logged a staggering 5,000 volunteer hours. During one of his first shifts, at age 14, he noticed an older woman crying in the waiting room. He watched as several nurses and doctors walked past her, undoubtedly needing to tend to patients. So, he sat down to see if she was all right and learned that her husband had been admitted to the emergency room the night before; she told him it had been the worst 24 hours of her life. Now, she was simply trying to go home and rest, but she couldn’t find where she’d parked her car. Boush helped her find her vehicle. It was a simple moment of connection and kindness that made Boush realize he wanted to work in health care. Now, working in community health, much of his role is listening to what people and communities need and seeing how the health system can be one part of a solution.
The Intervention
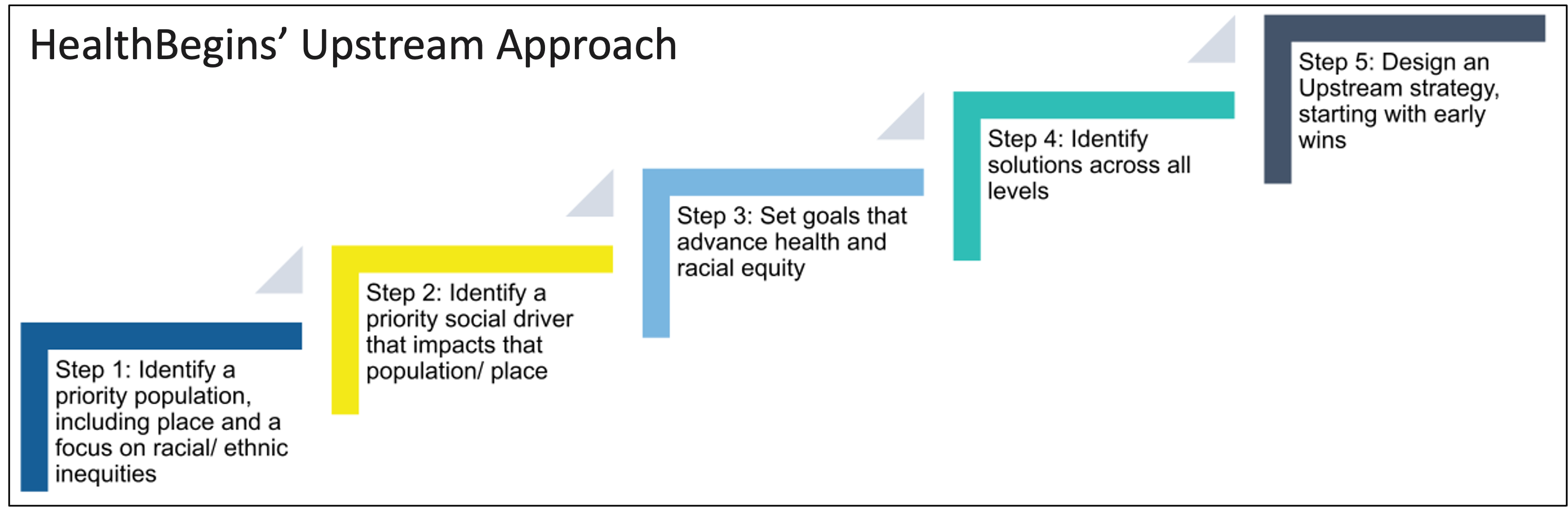
With the sudden pivot to ensuring vaccine access, Carilion applied some lessons learned from being part of HealthBegins’ Virginia Hospital and Healthcare Association (VHHA) Upstream Learning Collaborative. Carilion had initially joined the collaborative in 2019, focused on developing quality improvement initiatives to address social drivers that impact patients with diabetes. Boush and other Carilion leaders already understood the five steps in the Upstream Approach—identifying a specific population, identifying a need, setting goals, identifying solutions, and designing strategies—and these tools helped guide their new task with an equity lens.
After identifying the two specific neighborhoods with the lowest vaccination rates, Carilion turned to long-term community partnerships for help with the remaining steps. Over the last decade, staff from Boush’s department had developed close relationships with community leaders and organizations in the two priority neighborhoods while helping establish the Morningside Urban Farm, a Harvest Food Festival, and other food access projects. During the pandemic, Carilion relied heavily on those relationships to help identify barriers to vaccine access and specific strategies to overcome them.
Technology, transportation, and vaccine hesitancy proved to be the most significant barriers. Initially, appointments for mass vaccination clinics could only be booked online and required access to both a computer and the Internet. Appointments were filling up fast with people who had consistent internet access and the time to log on multiple times a day to try and book appointments. And the centralized downtown mass vaccination sites were harder to get to for people living in neighborhoods where transportation took longer and was less reliable.
The first step was working with city health officials to reserve a block of appointments in the online scheduling system that wouldn’t be available to the general public. Instead, those appointments were reserved for residents from the priority neighborhoods and could be booked directly by community leaders. Later, Carilion shifted toward a street medicine approach, where mobile care teams go into the community rather than ask residents to visit healthcare sites. It planned and hosted vaccination clinics at churches, community centers, and parks in both neighborhoods. It also hosted a community block party at a local pool where vaccines were made available, with masking and social distancing in place. These strategies aimed to deliver the vaccine in more inviting, community-based, easily-accessible environments.
All the various staff within Community Health and Outreach participated in planning and staffing these clinics. Community health workers leveraged the community relationships and trust they’d earned to identify locations for the clinics, build buy-in with community members, and develop confidence among the health educators and nurses staffing the clinics. Health educators assumed leadership roles in staffing and planning operations for the clinics, while nurses in the department administered the vaccines.
The Impact
Carilion and its partners vaccinated more than 100,000 people at the mega clinics, plus 2,770 individuals at 42 pop-up clinics in the priority neighborhoods through the street medicine approach. They were also able to attach other wraparound services—such as community health worker assistance, Healing Arts activities, and wellness and sun safety education—to the vaccine clinics, where health educators and community health workers could screen for and address other needs community members were experiencing.
Lessons Learned
COVID-19 will not be the last pandemic or major event that upends how health care is delivered and community health is approached. So when we don’t know the specifics of what will happen next or how needs will change, how can we prepare for what’s coming? Boush shared three lessons from Carilion’s vaccine equity work that the health system is carrying forward to help prepare for whatever comes next.
1) Long-term relationships in the community are critical to pivoting quickly in a crisis.
Relationships with community leaders and organizations are always central to designing effective upstream and health equity solutions. Input from community members is a critical tenet of HealthBegins’ Upstream Approach. However, building trust and meaningful relationships takes significant time and effort. And when needs arise rapidly, as they did during this pandemic, existing relationships were critical in being able to pivot and take a community approach to response. Without the existing relationships that Carilion developed through community development work over the last decade, none of the strategies implemented would have been possible.
Regular contact with other long-term partners was also how Carilion ensured it didn’t duplicate efforts to respond to community members’ needs during the pandemic. In partnership with the United Way, Carilion started Healthy Roanoke Valley in 2012. It’s a collective impact initiative with more than 50 nonprofit and local government partners working together to address needs identified in Carilion’s Community Health Assessments. The organizations in this group all shifted to COVID response during the pandemic. The initiative members met weekly to ensure that everyone had the same information about vaccinations and to coordinate the delivery of resources such as masks, sanitation wipes, and hand sanitizer to the community. The group continues to meet and is shifting to look at mental health issues as the pandemic continues.
2) Identifying and implementing effective interventions requires more integration, coordination, and communication among staff members internally.
Before the pandemic, nurses, community health workers, health educators, and peer specialists reported through Community Health and Outreach, yet each group worked on different projects without much coordination. The pandemic temporarily shifted the department’s focus to a handful of widescale urgent priorities that required an all-hands-on-deck approach. Everyone staffed vaccination clinics and assumed different leadership roles coordinating and doing outreach for those clinics. It forced staff members to leverage various skill sets, develop a deeper understanding of other team members’ roles, and create more robust communication within the department. Boush said that one of the essential takeaways from the pandemic is that the programs run by Community Health and Outreach need to be more deeply integrated—to improve access to specific services and better identify evolving needs and solutions.
As a starting place, Carilion is working with HealthBegins to better integrate the health education team and community health nurses into its community health worker program. “We know that when you’re working with a community health worker and when you’re starting to have behavior change, that you still might need some additional support to sustain that,” said Boush. “So we’re looking at how our health education team can come in and provide that health education, and then how our community health nurses can provide some of the preventive screenings and immunizations that might be needed.”
3) Having a consistent, proven tool to assess needs and identify solutions is critical—especially when you can’t anticipate the problem in advance.
Carilion was able to apply the five-step Upstream Approach learned through HealthBegins’ VHHA Upstream Learning Collaborative to help identify and implement solutions to several pandemic-related issues, including equitable vaccine distribution. The tool helped Carilion prioritize equity by asking staff to determine the communities with low vaccination rates and then center community voices and relationships to identify and plan community-based solutions for those populations. Having a proven set of steps and tools that Carilion previously used to design other interventions gave the health system a starting place and roadmap to approach this new work quickly.
Kate Marple is a Boston-based writer who specializes in helping nonprofit, health care, and legal services organizations develop practices to ensure that the stories they tell are shaped by and benefit people directly impacted by the issue(s) those stories are about. Her website is https://whotellsthestory.org.
Learn how HealthBegins can help you move healthcare upstream. Contact us to learn more.
Featured Content
Aligning Our Organizational Structure with Our Values
With our new B Corp Certification, HealthBegins has now joined a global network of companies that see business as a force for good and can share tools and practices to help us improve.
5 Principles and Practices to Sustain Gender-Affirming Care in Uncertain Times
With the onslaught of federal threats to transgender and nonbinary people, health care has a critical role to play to uphold standards of care, ensure access to essential services, advocate for evidence-based medicine, and protect patients and providers.
Strengthening Health Equity Investments with Human-Centered Stakeholder Engagement
Understanding and aligning with what value means to your stakeholders—especially those who make investment decisions—is crucial when making the business case for health equity investments.




