On April 24, we hosted a webinar entitled “Unmuddy the Waters: Healthcare and Social Services Integration.” This blog post summarizes and pulls from that event. If you missed it, you can watch the webinar here.
- Every system is a human system.
- Every problem is a communications problem.
Clinical-community partnerships and multisector collaboratives are now on the rise. However, stakeholders are using different terms and definitions when describing their values, work, and goals. This lack of clarity, precision, and agreement about the words we use make it harder to collaborate.
To address these issues, we recently held a webinar highlighting ways stakeholders in multi-sector collaboratives and clinical-community partnerships can better communicate about social determinants of health and health equity.
- Katherine Verlander of the Center for Medicare & Medicaid Services gave an overview of the Accountable Health Communities Model being led out of the CMS Innovation Center.
- Dora Hughes of The George Washington University discussed findings from the Funders Forum on Accountable Health.
- HealthBegins CEO Rishi Manchanda led a discussion about our newly released Upstream Communications Toolkit.
CMS’s Accountable Health Communities Model
The AHC Model is fundamentally testing three things:
- Systematic universal screening of all Medicare and Medicaid beneficiaries seeking care to identify unmet health-related social needs.
- Effectiveness of referrals and community service navigation on total cost of care using a rigorous mixed method evaluation approach.
- Partner alignment at the community level and implementation of a community-wide quality improvement approach to address beneficiary needs.
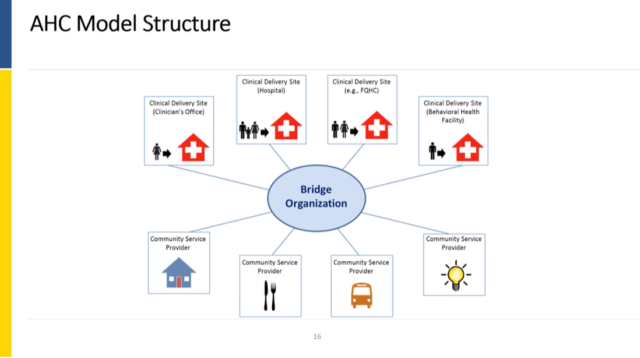
The AHC Model focuses on addressing health-related social needs (HRSNs), including housing instability, transportation, and food insecurity, among others. The model is designed to incentivize collaboration between the traditional health care system and the community-based organizations that are behind the health-related social needs of interest. This is good and important!
But these collaborations are exactly where the language confusion can come into play. And this is exactly where we hope communication tools can help unmuddy the waters.
GWU’s Funders Forum for Accountable Health
Our next presenter, Dora Hughes of The George Washington University, walked us through the Funders Forum for Accountable Health, a group funded by both private and public organizations. The Forum came together in part because the funders were funding various organizations to advance multi-sector collaboratives, sometimes known as “Accountable Communities for Health,” but in a siloed fashion and without a shared framework for communicating and evaluating efforts. The Forum set out to do four things:
- Convene public and private funders of Accountable Communities for Health (ACH)
- Share learning and facilitate collaboration
- Identify priorities for evaluating ACH impact
- Explore options for supporting the ACH Model
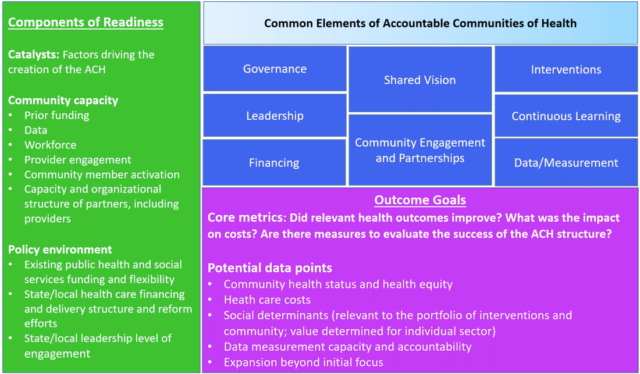
Including the 31 sites mentioned by Katherine, Dora and her team believe that 100 sites across the country can be loosely classified as “Accountable Communities for Health.” While their exact structures and scopes of work vary—some are deeply integrated with health care delivery whereas others are much more community-based and others a mix of the two—their general goals and vision are the same. (The common elements defining Accountable Communities for Health are outlined in the blue-boxes of the image above, a slide pulled from Dora’s presentation.)
There’s quite a range of experiences and lessons learned emerging from these efforts. And to help communicate those stories, the Forum will be releasing 10 in-depth case studies later this year.
But one thing they have seen is ACH struggle with communication, not just between the health care and the social sectors within communities, but also across the different ACH communities. An ACH in California may be using different words to describe their work than an ACH in Texas. Particularly in regard to the financial side of the lexicon: What is “value?” What is “return on investment?”
Dora herself remarked that the CMS “Accountable Health Communities (AHC)” model and the “Accountable Communities of Health (ACH)” were confusingly similar terms. These language issues make conversations across this work challenging. They can hinder the overall progress of the field.
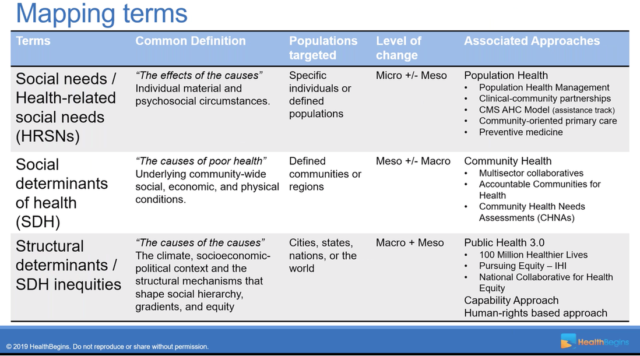
The way we see it, CMS AHC sites are focused primarily on addressing individual-level social needs while those involved in broader ACH efforts often seek to address community-level social determinants of health.
The HealthBegins Communications Toolkit: Glossary, Framework, and Discussion Guide
- Health-Related Social Needs: are “the effects of the causes.” HRSNs—as they’re usually acronymed —focus on individual needs. A diabetic patient with food insecurity needs food. An unhoused individual comes into the ER, that person needs a house.
- Social Determinants of Health: are “the causes of poor health.” This is the most commonly known phrase, but is often used too loosely. SDHs can be thought as general community-level and community-specific issues. The issues may have the same names of HRSNs—housing and food insecurity for example—but the analysis and interventions go beyond the individual.
- Structural Determinants: are “the causes of the causes.” These are the inherent structures that have long driven health inequalities in society. Larger issues like racism, sexism, gender issues, and wealth inequality.
Importantly, the Glossary is not meant to be set in stone; it’s a living document, meant to simply offer a starting point to help people understand each other.
The second part of the Toolkit is a Levels of HRSN & SDH Integration Framework. A more sophisticated tool, the Integration Framework is designed to help healthcare and social service partners apply the Glossary of Upstream Terms in their own settings. It helps partners find and clarify a shared set of goals, priorities, and approaches to collaborating.
The third part of the Toolkit is a simple Discussion Guide. This Guide helps healthcare and social sector leaders take commonly used terms to create a shared, living language for partnership and collaboration. The Guide provokes partners to consider fundamental challenges—like how to balance financial and social returns and how to avoid “medicalizing” social services. It also provokes each partner to consider the role that each can play in addressing “the causes of the causes,” i.e. the structural determinants like racism and income inequality.
You can find the toolkit on our Resources for Social Determinants of Health page. This Toolkit is in an early form that is up for discussion. We welcome your thoughts, questions, and comments. Just reach out to us and we’d be happy to set up a conversations around this.
Closing Discussion and Thoughts
This is messy stuff! It’s going to take deliberate effort and significant time before things shape into something even close to seamless.
We will never reach a place where we all understand each other perfectly and easily the first time. There will always be communication problems to work out along our collective journey upstream.
All in all: We hope this helps umuddy the waters just a bit.
Featured Content
Staff Spotlight: Alejandra Cabrera, Perfectly Imperfect Artist and Health Equity Advocate
When I work with people and communities, I always think back to this sense of not belonging and it drives me to continue to do the heart-work we need to do to advance health equity.
Staff Spotlight: Ellen Lawton, Pioneer of Medical-Legal Partnership
“There should be a lawyer, a legal aid lawyer, in every single clinic in the country. You don’t have to call them a legal aid lawyer. You can call them a problem solver.”
Staff Spotlight: Taleen Yepremian, Determined to End Inequities in Health Care Access
“It was heartbreaking to see kids that can't see a doctor or can't see psychologists or any type of provider they need because they don't have the insurance, they don't have the access to care.”


